What is Shoulder Cartilage Restoration?
Shoulder cartilage restoration refers to a group of procedures aimed at repairing or regenerating damaged cartilage in the shoulder joint, especially the glenohumeral (ball-and-socket) joint. Cartilage damage in the shoulder can result from injury, osteoarthritis, or degenerative wear, leading to pain, stiffness, and loss of function. Shoulder cartilage restoration procedures help to reduce pain and inflammation, restore a more normal range of motion and function, stabilize the joint, and reduce the risk of further cartilage damage.
Types of Shoulder Cartilage Restoration Techniques
Some of the common shoulder cartilage restoration techniques include:
- Microfracture: In this technique, tiny holes are drilled into the bone beneath the cartilage defect to stimulate a healing response and formation of fibrocartilage. This technique is best suited for small, contained defects.
- Osteochondral Autograft Transplantation (OATS): In this technique, a plug of healthy cartilage and bone is taken from a non-weight-bearing area and transplanted into the area of defect. This technique is best suited for small to moderate defects.
- Osteochondral Allograft Transplantation: This technique involves the use of cadaveric donor cartilage and bone to fill large defects. This technique is suitable for large or complex cartilage lesions.
- Autologous Chondrocyte Implantation (ACI): In this technique, cartilage cells are harvested from the patient, cultured in a lab, and then implanted into the defect. This technique is suitable for larger focal cartilage lesions.
- Biologic Augmentation (e.g., PRP or stem cells): This is a nonsurgical treatment in which platelet-rich plasma (PRP) or stem cells are injected into the shoulder to promote cartilage healing or reduce inflammation. This method is best suited for early-stage cartilage degeneration.
- Arthroscopic Debridement and Chondroplasty: This technique involves smoothing frayed cartilage and removing loose fragments, primarily through arthroscopy.
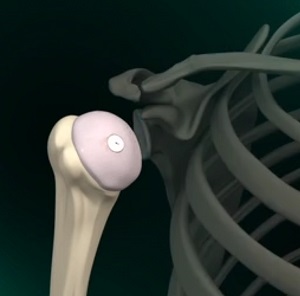
Shoulder Anatomy
The shoulder is a highly movable body joint that allows various movements of the arm. It is a ball-and-socket joint, where the head of the humerus (upper arm bone) articulates with the socket of the scapula (shoulder blade), which is called the glenoid. The two articulating surfaces of the bones are covered with cartilage, which prevents friction between the moving bones. Tendons and ligaments around the shoulder joint provide strength and stability to the joint.
Indications for Shoulder Cartilage Restoration
Common indications for shoulder cartilage restoration include:
- Focal cartilage defects (not widespread arthritis) in the humeral head or glenoid
- Persistent shoulder pain not relieved by conservative treatment, like rest, physical therapy, or injections
- Mechanical symptoms like catching, locking, or grinding
- Young or active patients aiming to delay or avoid shoulder replacement
- Post-traumatic cartilage injury or cartilage loss from shoulder instability or dislocation
- Good overall joint alignment and stability, without severe bone loss or deformity
Procedure for Shoulder Cartilage Restoration
Shoulder cartilage restoration is typically performed under general anesthesia, using either an arthroscopic (minimally invasive) or open surgical approach.
- Arthroscopic approach: An arthroscope - a small, fiberoptic instrument consisting of a lens, light source, and camera at its end is used for minimally invasive access. The camera projects images of the inside of the joint onto a large monitor, allowing your surgeon to assess the cartilage damage and perform the repair using tiny surgical instruments.
- Open surgery: This involves making a larger incision over the joint to assess the cartilage damage and perform cartilage repair/restoration. This approach is typically employed if the damage is extensive or if grafting is needed.
Once the treatment area is accessed, the surgeon begins by assessing the extent of cartilage damage in the glenohumeral joint. For small defects, microfracture is often used - this involves creating tiny holes in the bone beneath the damaged cartilage to stimulate the formation of new fibrocartilage. In cases of larger or deeper defects, the surgeon may perform an osteochondral autograft or allograft transplant, where healthy cartilage and bone are transferred to the damaged area. Chondroplasty may be done to smooth frayed cartilage edges, and biologic treatments like platelet-rich plasma (PRP) or stem cell injections may be added to enhance healing. Once the restoration is complete, the wound is closed, and a sterile bandage is applied.
Postoperative Care and Recovery
Postoperative care following shoulder cartilage restoration focuses on protecting the repair, managing pain, and gradually restoring shoulder function. Initially, the arm is placed in a sling for several weeks to limit movement and allow healing. Pain is managed with medications and cold therapy. Passive range-of-motion exercises typically begin early under the guidance of a physical therapist to prevent stiffness without stressing the repaired area. As healing progresses, active movements and strengthening exercises are gradually introduced over the next few months. Full return to sports or heavy activities is generally delayed for 4 to 6 months, depending on the procedure performed and the patient’s recovery progress.
Risks and Complications
Shoulder cartilage restoration is generally safe, but like any surgical procedure, it carries certain risks and potential complications. These include:
- Infection
- Stiffness or loss of motion
- Graft failure
- Persistent pain
- Blood clots
- Nerve or vessel injury
- Delayed healing
For more information about our services or to schedule an appointment, call us at / or click here to request an appointment online. We’ll respond to you as soon as possible.